Researchers Develop Non-Addictive Painkiller Targeting Chronic Pain Sites
TEHRAN (Tasnim) – Scientists have designed a groundbreaking painkiller that activates solely at chronic pain sites, offering targeted, non-addictive relief.
Researchers have engineered a new painkiller that remains dormant until it reaches areas of chronic pain, diverging from traditional analgesics that broadly dull nerve signals.
The team behind this compound aims to begin human trials, marking a significant step forward in chronic pain management.
Unlike standard medications, this innovative drug is a prodrug, which stays inactive until specific biological conditions trigger it within the body.
Prodrugs are advantageous because they deliver medication precisely where it's needed, reducing side effects.
Leveraging a known chemical reaction, an international research team has designed this drug to provide targeted pain relief, particularly for chronic pain patients.
"Our team has created a targeted prodrug capable of relieving chronic pain during preclinical trials," said Professor Andrew Abell from the University of Adelaide, co-corresponding author of the study.
"We believe we were the first to apply this particular chemical reaction in a biological setting, and we foresee its potential for other applications."
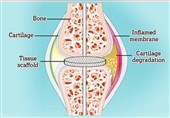
This prodrug activates upon contact with reactive oxygen species (ROS) like hydrogen peroxide, which exist in higher concentrations at chronic pain sites.
The compound circulates through the body, remaining inactive until it encounters these ROS-rich areas, where it then delivers its pain-relieving effects.
"Existing chronic pain drugs only help about one in six people by reducing nerve activity," explained Associate Professor Peter Grace from the University of Texas MD Anderson Cancer Center, the study's other co-corresponding author.
"Our new prodrug tackles an underlying issue by reducing molecules responsible for sending pain signals, opening a new path for chronic pain treatment."
The researchers tested the prodrug on mouse models with localized oxidative stress, a hallmark of chronic pain conditions.
In tests on diabetic neuropathy, osteoarthritis, and chemotherapy-induced peripheral neuropathy models, the prodrug reversed sensitivity to touch and cold six months post-injury.
The study found that while the effects were dose-dependent, consistent dosing sustained the pain relief without building tolerance, unlike opioid painkillers.
"This result showed the compound did not induce tolerance, a major limitation of opioids like morphine," said Dion Turner, a PhD candidate and co-author.
"Chronic pain remains a significant unmet need, and non-addictive options like this could revolutionize the field currently dominated by addictive opioids."